The Public Health Officials Say “Trust Us.”
The Public Health Officials Say "Trust Us." The Data Says Otherwise.
I hate to be the bearer of bad news, Ben Shapiro, but feelings trump facts when it comes to covid-19. This is thanks entirely to the love triangle forged between the corporate press, government officials, and tech giants whose sinister and divisive campaign of fear and censorship spawned a reaction so virulent that society was upended in a matter of weeks for a virus with a 99 percent plus survival rate.
In no time whatsoever sacrificing for and preserving “public health”—costs be damned—became the chief end of mankind. Relegating oneself to a life of unquestioned submission to lockdowns and mask mandates became the greatest calling one could fulfill—at least until the vaccine arrived.
As our most fundamental human rights were stripped away, did any president, prime minister, governor, or mayor suggest that maybe “the people” have a vote to determine whether or not every aspect of their lives should be subject to manipulation on a daily basis? Of course not. As it turns out, your “sacred right to vote” may only be exercised so long as the ruling class permits. It appears that our only job in times of emergency is to wait for marching orders from those with political power.
What many should have come to realize over this past year and a half are two lamentable impulses of the average person: (1) the trained instinct, learned primarily in government schools, to revere and please those in positions of perceived authority and (2) the desire for safety over liberty. Fused with modernity's cushy standards of living, these two traits enabled a series of effortless goalpost shifts, starting from “We’re all in this together!" to “Three jabs or weekly testing, else you and your family can starve.” Mind you, anybody who predicted far less draconian policies in the early stages of the pandemic was promptly labeled a conspiracy theorist.
At their core, these pandemic schemes—lockdowns, curfews, capacity restrictions, vaccine mandates, and more—relied heavily on a blind trust in the ruling elite’s public health pronouncements and our desire to behave in a socially approved, conflict-free manner. But as it turns out, all of the big-picture covid data from the past eighteen months regarding lockdowns, and vaccine uptake thoroughly implicate the ruling elite.
The Covid-19 Data We Need to Accept
There is zero meaningful correlation between lockdown strength and covid-19 outcomes.
Prior to 2020 lockdowns had never been recommended as a public health response, even for severe respiratory outbreaks. However, with a little bit of media-induced panic, social pressure, and a theistic reverence for computer modeling, it was quickly accepted that these historically and scientifically unprecedented public health measures saved lives. In turn, it was simply agreed that more stringent lockdowns would be more effective than weaker lockdowns.
All costs and moral arguments aside, heavy skepticism toward lockdowns was justified as early as April 2020, when it was shown that a region's time to lock down made no impact on its death toll.
Fast-forward eleven months and we find that data from March 1, 2020, to March 1, 2021, show that lockdowns were always a nonfactor in mitigating the spread of covid-19. The following data was split into four three-month periods to better account for changes in each nation’s stringency index. The period of measurement was cut off on March 1, 2021, to exclude any significant vaccine uptake. Because Israel was the only nation in the following graph that had significant full vaccination rates going into March 2021, it has been excluded from the last period of measurement.
Source: Our World in Data COVID-19 dataset (stringency_index, total_cases_per_million, total_deaths_per_million).
Quite plainly, more stringent lockdowns, regardless of population density—illustrated by the size of the dots—had no greater effect on covid-19 outcomes than less stringent lockdowns. In fact, the minimal correlation that does exist slopes in the opposite direction of what we’ve been trained to believe about lockdowns.
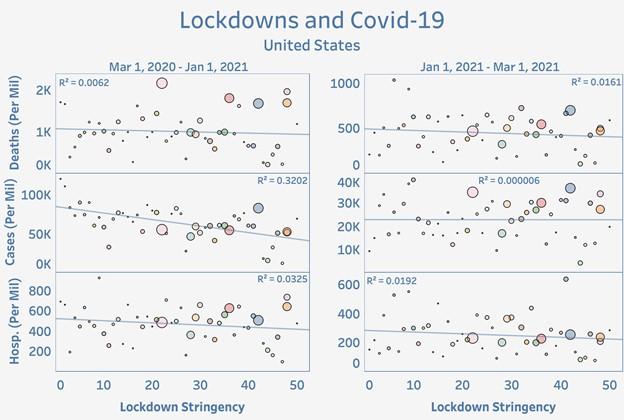
Similar conclusions can be drawn about lockdowns in the United States. Due to data constraints on lockdown stringency, the following state data is broken down into two periods: one much larger period extending from March 1, 2020, to January 1, 2021, and a second period extending from January 1, 2021, through March 1, 2021.
Source: Data on cases and deaths from Our World in Data COVID-19 dataset (total_cases_per_million, total_deaths_per_million); data on hospitalizations from HealthData.gov (COVID-19 Reported Patient Impact and Hospital Capacity by State Timeseries); data on stringency for January 2021–March 2021 from Adam McCann "States with the Fewest Coronavirus Restrictions," Wallethub, Apr. 6, 2021; and through Dec. 31, 2020, from Laura Hallas, Ariq Hatibie, Saptarshi Pyarali, and Thomas Hale, "Variations in US States' Responses to COVID-19" (BSG Working Paper Series BSG-WP-2020/034, version 2.0, University of Oxford, Oxford, UK, December 2020). Data on population density from World Population Review (US States – Ranked by Population 2021).
Again, we find no statistically significant correlations between lockdown stringency and cases, deaths, or hospitalizations. Population density, again noted by the size of the dots, was also a nonfactor.
Quite plainly, no matter the intensity, duration, or location of the lockdown mandated by government authorities, no respiratory virus can be legislated away. The claims that lockdowns are some sort of life-saving public health measure and that the strength of a region’s lockdown is inversely related to covid-19 incidence is simply not borne out in the data.
Briefly I would like to note one glaring cost of lockdowns based on recent Centers for Disease Control and Prevention (CDC) estimates, namely the abnormally high level of drug overdoses that have persisted since the first half of 2020.
Source: Data.CDC.org (Early Model-Based Provisional Estimates of Drug Overdose, Suicide, and Transportation-Related Deaths).
While there are many more costs associated with lockdowns than can be discussed in one article, it is important to realize that even if the lockdowns were costless, their inefficacy is enough to render them useless as a public health measure.
Hospitals, on the whole, were never overrun.
While it is tempting to generalize based on a few extreme cases that exist at the tail ends of a distribution, these cases are not representative of the whole. This temptation is succumbed to most frequently when manufacturing panic about overrun and overcrowded hospitals. While these stories are seemingly endless, they are nevertheless statistical outliers. A brief review of United States hospitalization data confirms as much.
Source: HealthData.gov (COVID-19 Reported Patient Impact and Hospital Capacity by State Timeseries).
From consuming corporate press headlines one may have the impression that just about every hospital is operating above or near 100 percent capacity. As it turns out, inpatient bed utilization—these are staffed inpatient beds that include all overflow and surge/expansion beds used for inpatients, including all ICU beds—across the United States has stayed below 76 percent over the course of the pandemic while inpatient bed utilization for covid-19 patients has never surpassed 15 percent. However, judging by the fact that the 2021 seasonal summer surge—which has already peaked—has surpassed the 2020 seasonal summer surge, these rates will likely be exceeded when the deadlier seasonal winter surge arrives in the coming months. Nevertheless, it would be mere speculation to suggest that hospitals are going to exceed or reach nearly 100 percent capacity as winter rolls around.
While 76 percent utilization may seem high, former medical director James Allen points out that an 85 percent occupancy rate is commonly considered to be optimal operating capacity. Allen remarks that having too small of an occupancy rate means that workers and resources are sitting idle, which can lead to layoffs. On the other hand, a near–100 percent occupancy rate would be too much of a strain on resources, leaving patients without care.
While there are certainly extreme cases of hospitals being pushed beyond capacity, the idea that United States hospitals, on average, have been operating at or beyond 100 percent capacity is absolutely ludicrous.
Vaccine uptake is not preventing case growth.
The covid-19 vaccine just may be the most hyped pharmaceutical product in medical history. Marketed to the world as nothing short of global salvation, the vaccine was supposed to kickstart our return to normalcy. Despite this belief, the data suggest that increased vaccination rates are failing to slow the spread of covid-19.
First, let’s assess the following claim made by Anthony Fauci during a June 3 CNN interview: "When you’re below 50 percent of the people being vaccinated, that’s when you’re going to have a problem . . . With 50 percent vaccinated I feel fairly certain you're not going to see the kind of surges we've seen in the past.” Mind you, if Fauci believed that 50 percent vaccination rates were going to halt surges, you can bet a majority of the nation felt the same way.
Source: Data on cases from Our World in Data COVID-19 dataset (new_cases_smoothed_per_million); data on vaccination rates from Data.CDC.gov (COVID-19 Vaccinations in the United States Jurisdiction).
As you can see, mere weeks after 50 percent full vaccination rates had been achieved in twenty states, cases in each one of those states erupted. It comes as no surprise that authorities are now calling for 70, 80, or 90 percent vaccination rates to get things under control.
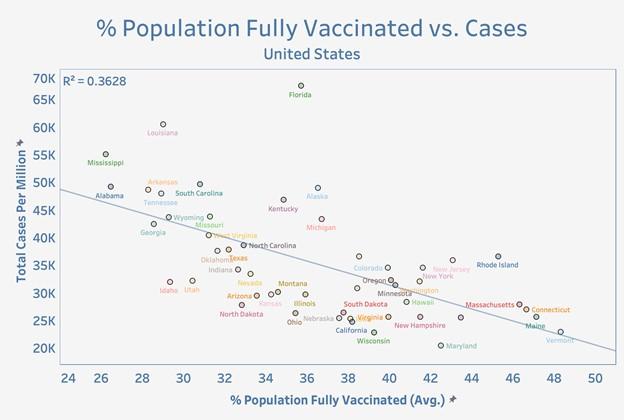
Looking at the entirety of the United States since March 1, 2021, there is no statistically significant indication that states that have administered, on average, more vaccine doses are faring any better than states that have administered fewer doses on average.
Source: Data on cases from Our World in Data COVID-19 dataset (total_cases_per_million); data on vaccination rates from Data.CDC.gov (COVID-19 Vaccinations in the United States Jurisdiction). Date range is Mar. 1, 2021–Sept. 9, 2021.
Moving along to full vaccination rates, there is again no statistically significant indication that states and countries with higher percentages of their population fully vaccinated are mitigating case growth any better than states with lower percentages of their population fully vaccinated. As before, fully vaccinated rates are taken as an average of the past six months.
Source: Data on cases from Our World in Data COVID-19 dataset (total_cases_per_million); data on vaccination rates from Data.CDC.gov (COVID-19 Vaccinations in the United States Jurisdiction). Date range is Mar. 1, 2021–Sept. 9, 2021.
Source: Data on cases and vaccination from Our World in Data COVID-19 dataset (total_cases_per_million, people_fully_vaccinated). Date range is Mar. 1, 2021–Sept. 9, 2021.
Additionally, a recent vaccine surveillance report from the UK shows that fully vaccinated individuals between the ages of forty and eighty are getting infected at higher rates than their unvaccinated counterparts. For those under forty and over eighty, infection rates among the vaccinated are lower than in the unvaccinated, but still significant.
Source: Public Health England, COVID-19 Vaccine Surveillance Report – Week 36 (London: Public Health England, 2021).
If this isn’t enough to raise some eyebrows, there are plenty of instances of countries—only a few shown below—having experienced a surge in cases or even their highest case levels of the pandemic amid ever-increasing rates of vaccination.
Source: Data on cases and vaccination from Our World in Data COVID-19 dataset (new_cases, people_fully_vaccinated).
Keep in mind that the percentage of people who have received at least one dose is higher than what’s displayed above. So the assumption that simply getting jabs out to people—not having to fully vaccinate them—was going to bring cases to a screeching halt is also incredibly dubious.
Pertaining specifically to the month of August, we find that a number of highly vaccinated nations are experiencing worse total case numbers amidst the highly vaccinated summer of 2021 as opposed to the unvaccinated summer of 2020.
Source: Data on cases and vaccination from Our World in Data COVID-19 dataset (total_cases_per_million, people_vaccinated).
How can it be the case that a 0 percent vaccinated country had far fewer cases last year than it did once 60, 70, or 80 percent of its population was fully vaccinated with what is professed to be an incredibly effective vaccine? Why, despite these far worse metrics, are we no longer seeing the strict lockdown measures like business closures, curfews, capacity restrictions, or stay-at-home orders that defined the summer of 2020? Collegiate and professional sports arenas that were empty just one year ago are now packed to the brim; and little to no effort is being made to check for vaccination status or proof of negative test at the gate. Are we seriously expected to believe that our political leaders have any desire to preserve the “public health” when they’re allowing their economies to operate with practically no mitigation measures in place despite climbing metrics? Maybe you are starting to realize that these “public health” measures and the new vaccine mandates never had anything to do with your health.
Despite all the data we have on lockdowns, hospitalization trends, and newly emerging vaccination data, one can only marvel at how trust in the public health system and ruling elite can persist in any capacity.















Post a Comment